
The report titled “Uninspected and Neglected” by the majority staff of the US Senate Special Committee on Aging brings attention to a pressing issue: the severe understaffing of inspection agencies causing significant delays in surveys. While some providers may temporarily appreciate the respite from annual surveys, this situation exacts a heavy toll on providers and, more alarmingly, jeopardizes the well-being of residents and potential residents.
These consequences underscore not only the urgency in addressing staffing challenges within inspection agencies, but also the compelling need for comprehensive reform within Centers for Medicare & Medicaid Services programs reliant on survey data. This reform is imperative to ensure fair, accurate and timely assessments that prioritize the safety and care standards crucial for nursing home residents and providers.
The consequences stemming from delayed surveys impact the financial landscape as well. For many nursing homes, surveys represent an avenue for impartial third-party feedback, which they integrate into their Quality Assurance and Performance Improvement (QAPI) processes. However, the flip side reveals a concerning reality: Past poor survey results, which never expire, exert lasting repercussions. These repercussions include less ability to refinance, loan defaults, exclusion from preferred networks, and diminished Five-Star ratings — which subsequently result in decreased occupancy rates.
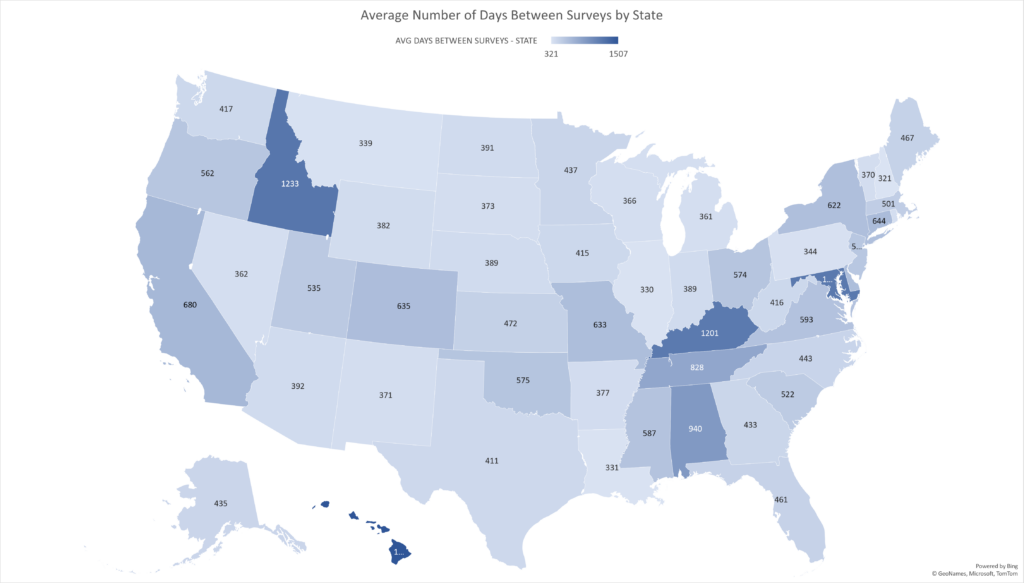
Taking a bird’s-eye view, significant variations exist in the intervals between annual surveys and certifications across states. In New Hampshire, the average stands at a low of 321 days, while Hawaii reports the highest at a staggering 1,507 days. The national average falls at 530 days, with a few alarming outliers (Idaho, Kentucky, Maryland) in the 1,000-plus day range.
However, another concern lies in the incomplete narrative presented by these averages. State-based survey teams cover specific geographic areas, and survey timelines are often inconsistent across those areas, which is reflected within states. As an example, Massachusetts has a statewide average of 501 days between surveys. Yet examination at county levels reveals substantial discrepancies: Plymouth County records an average of 768 days between surveys, while Suffolk County experiences significantly shorter intervals at 357 days.
As highlighted in my previous report in McKnight’s Long-Term Care News, the occupancy rates in nursing homes exhibit a direct correlation with Five-Star ratings, and the Health Inspection component plays a pivotal role, essentially “wagging the dog” within the Five-Star system. A negative survey doesn’t just result in immediate repercussions; it has a prolonged impact due to the extended lag time between surveys.
Consider this: Distressed nursing homes often undergo acquisition and implementation of a “turnaround” team striving to enhance staffing, clinical outcomes and compliance. Despite measurable improvements in these areas, often reflected quarterly on Medicare.gov, their efforts encounter a roadblock. They face an agonizing wait for a new survey to uplift their Health Inspection rating. However, the waiting period for a new survey paints a starkly different picture across states: Virginia at 600 days, California at 680 days, and Maryland at an alarming 1,205 days.
One might reasonably assume that nursing homes on the Special Focus Facility (SFF) candidate list would undergo more frequent surveys. However, reality paints a different picture. Despite being on the proverbial “watch list” as SFF candidates, facilities in 37 states face, on average, an additional 90 days of waiting compared to non-candidate facilities. Shockingly, in 10 states, SFF candidates endure survey intervals over 200 days longer than their non-SFF candidate counterparts.
This discrepancy in survey frequency feels like not only an added punitive measure, but also a discouragement against prioritizing and enhancing quality improvement initiatives. The extended waiting period for surveys in SFF candidate facilities seems contradictory to the intended purpose of the designation.
I am urging CMS to critically assess the impact of staffing shortages on the nursing home industry, both in terms of quality of care and financial viability. I strongly advocate for a reconsideration of the Health Inspection domain calculation when survey intervals exceed 365 days. One potential solution is to reassess the inclusion of the oldest survey cycle and either replace it with the state average or utilize data from cycle one and cycle two exclusively.
Another consideration could involve reevaluating the entire Five-Star rating system, perhaps by temporarily suppressing the Health Inspection rating to avoid consumers misattributing a poor showing to the nursing home provider rather than the state agency. It’s imperative to ensure that any adjustments maintain clarity and accurately reflect performance without making unsubstantiated suggestions of subpar nursing home quality.
The fundamental question that demands attention is the correlation between survey results and the actual quality of care provided in nursing homes. While the Five-Star Health Inspection and Quality Measure domains exhibit little or no correlation, it’s crucial to explore other metrics that may more accurately depict quality.
The pressing inquiry revolves around determining the optimal survey interval. Are annual surveys sufficient to drive improved outcomes? Government agencies often assert that extended survey intervals lead to compromised care, yet we seem to lack empirical evidence to substantiate this claim. The absence of analytical insights in this realm is striking, given the wealth of available data that could guide our understanding.
We face a gap in analysis that could serve as a beacon to navigate these critical questions. There’s a substantial need for comprehensive research to decipher the true relationship between survey results and the quality of care provided in nursing homes.
Steven Littlehale is a gerontological clinical nurse specialist and chief innovation officer at Zimmet Healthcare Services Group.
The opinions expressed in McKnight’s Long-Term Care News guest submissions are the author’s and are not necessarily those of McKnight’s Long-Term Care News or its editors.
Have a column idea? See our submission guidelines here.




